The timing and appropriateness of surgery of the hand and arm in children with birth anomalies are difficult topics. The problem for parents and doctors is that we don't truly know how well any particular child will adopt to his limitations and how much those limitations will affect his/ her life. We all hope for kids with excellent function and 'normal' appearance and, therefore, families seek doctors and surgery to make their kid's hands 'normal'. As a surgeon with experience, I see it as my job to share
reasonable expectations about surgery (as well as risks and recovery).
As kids get older, they can participate in decision- making. But the reality is that families often want 7 year old or 10 year old kids to really make the touch decisions about whether to have surgery and that is not likely to be helpful. We want such kids to have a stake in the decision but they are not usually able to truly really make such difficult decisions. Understanding the future is tough and having reasonable expectations about surgery (pain, recovery, etc) is really challenging. In the case below of a 17 year old, his feelings and his life experience with his condition are vital to an appropriate decision for surgery (in this case family was interested and he was absolutely not).
These are issues that we face
every day in clinic and every family approaches such decisions differently. It is my job to help each family, in its different way, make the best decision. Not easy (and sometimes talking through this is more challenging than the surgery itself).
Distal arthrogryposis is, in my practice, less common that
amyoplasia or the more extensive disease. Because the disease is focused on the hands alone, patients tend to function at a higher level and have an easier time with activities in general. I have posted twice on this topic,
here and
here. Surgery is often considered as it can improve hand position and sometimes finger and thumb motion. But such decisions are not easy for most families.
I recently met a 17 year old male who reminded me that function can be very good even with some deformity and some limitations in motion. He was absolutely not interested in surgery as he felt he could perform all activities without too much difficulty. He did admit to using two hands for activities that others would accomplish with only one hand. He also stated that some tasks might take him a bit longer to complete compared to other kids. But he was not interested in surgery.
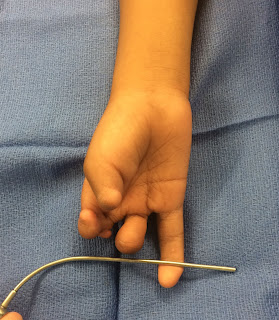
Here are some pictures of his hand (both sides looked the same) to frame the discussion. The fingers do not straighten fully, especially the ring and small fingers with camptodactyly. The fingers do however make a great fist (which is not always the case in other types of arthrogryposis) and with some strength. Finally, the thumb web space is only marginal, not great, which limits his ability to grab larger things.
![]() |
| Distal arthrogryposis with attempted finger straightening |
![]() |
| Distal arthrogryposis with attempted finger straightening from palm view |
![]() |
| Distal arthrogryposis with a full fist demonstrated |
Obviously, we did not perform surgery on this happy 17 year old with imperfect hands. His parents were somewhat interested in learning more about the options which included therapy to help straighten the fingers (vs surgery to release the tightness on the palm side) and possibly surgery to help the thumb web space. But could do everything he wanted to do and was okay with accomplishing certain goals differently than his peers.